Dr. Raj Arora is dedicated to empowering his patients with knowledge about their eye health and available treatment options. As a Board-Certified Optometrist, he takes a personalized approach to care, ensuring each patient fully understands their condition and the best solutions for their vision needs.
Dr. Arora specializes in custom specialty contact lenses designed to manage complex eye conditions, including:
✔ Keratoconus
✔ Pellucid Marginal Degeneration
✔ Post-RK Complications
✔ Severe Dry Eyes
✔ Blepharitis
With his expertise in advanced contact lens technology, Dr. Arora provides tailored solutions to improve vision clarity, comfort, and overall eye health. Whether you’re seeking specialized care or exploring new vision correction options, Dr. Arora is committed to delivering exceptional, patient-centered optometric care.
Keratoconus
Keratoconus is a progressive eye condition where the cornea thins and bulges into a cone shape, causing blurred or distorted vision. This irregular shape prevents light from entering the eye correctly, making traditional glasses less effective. At Nusight Vision, Dr. Raj Arora specializes in diagnosing and managing Keratoconus. Dr. Arora customizes treatment plans using advanced diagnostic tools like corneal topography, including specialty contact lenses such as rigid gas permeable, scleral, and hybrid lenses to help improve vision. Dr. Arora also offers Corneal Cross-Linking for patients in the early stages to halt progression and preserve corneal integrity.
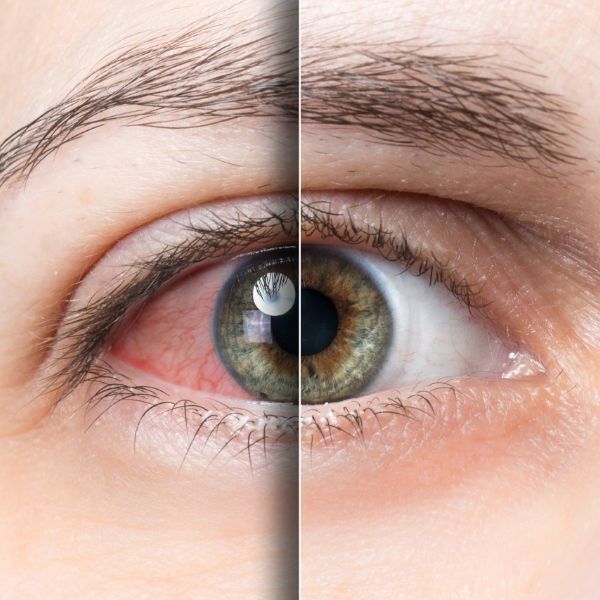
Keratoconus is a slow-progressing condition where the cornea—the clear, dome-shaped front of the eye—thins and bulges into a cone shape. This irregular shape distorts light entering the eye, causing blurry or distorted vision that glasses cannot correct.
What causes Keratoconus?
As of 2020, the exact cause of Keratoconus remains unknown. However, several factors may contribute to its development, including:
Keratoconus can develop at any age but often begins in the late teens or early 20s, progressing over several years. It typically affects both eyes, causing persistent distorted vision and nighttime glare, even with updated glasses. Frequent increases in myopia and astigmatism may also indicate its presence.
Optometrists are often the first to detect Keratoconus through a detailed evaluation of the cornea. The gold standard for diagnosis is corneal topography—an advanced imaging technique that maps the curvature and thickness of the cornea.
At Nusight Vision, we use the TopCon CA-800 Corneal Topographer, a state-of-the-art device capable of detecting even the most minor changes in corneal shape. Our system includes a built-in Keratoconus Screening Tool, enhancing the accuracy and reliability of our diagnosis.
Secondly, doctors view the cornea through a microscope and evaluate the presence of corneal thinning or irregularities indicative of Keratoconus.
In the early stages of Keratoconus, glasses or soft contact lenses may provide sufficient vision correction. As the condition progresses, specialty lenses—such as rigid gas permeable, scleral, or hybrid lenses—offer clearer, more comfortable vision. In severe cases, a corneal transplant may be required.
If Keratoconus is diagnosed early and shows signs of progression, Corneal Cross-Linking can help halt its advancement. Approved in the U.S. in 2016, this procedure uses riboflavin (vitamin B2) eye drops activated by UV light to strengthen corneal collagen fibers and prevent further bulging or thinning.
